A DAN Boater Travel Health & Safety Guide
We all hope to never experience a serious emergency while we are traveling. But chances are that some travelers will face a problem — and sooner or later that traveler may be you. The better informed and prepared you are for such an event, the less likely you are to suffer serious consequences.
In this guide, you'll learn about:




Plane crashes and shipwrecks make headlines, though the odds of experiencing such an event are minuscule. Many other hazards are associated with various modes of travel. Luckily for travelers, those other risks are often ones you can do something about.

Flying exposes travelers to high altitudes, a decreased level of oxygen, relatively quick changes in atmospheric pressure during ascent and descent, dry air, and adjacency to other travelers who may be carrying transmissible diseases.
Major passenger airliners typically cruise at 36,000 feet and maintain cabin pressure at a level equivalent to 5,000 to 8,000 feet. At that pressure, oxygen in the cabin air is reduced to about 80 percent of what is present in the atmosphere at sea level. This may affect people with severe lung, heart or circulatory diseases. If you have such a condition, be sure to consult your physician before you travel by air.
During ascent and descent, the cabin pressure changes relatively quickly. If gas is unable to move freely in or out of your middle ears and sinus cavities, a pressure differential may occur, which can cause pain in your ears or sinuses. For this reason, it is important to remain awake while your plane ascends and descends and to actively equalize the pressure in your ears. Chewing gum will naturally make you equalize without any pharmacological aid. If you are congested or suffer from excessive postnasal drip, check with your physician or pharmacist to see if it is safe for you to take an over-the-counter decongestant (or a similar prescribed medication) to help keep open your sinus passages and to improve your ability to equalize your middle-ear pressure.

Long transmeridian flights can also result in greater-than-usual fatigue. The more time zones you travel through, the more likely you are to experience the well-known phenomenon of jet lag. People traveling from the northern to the southern hemisphere (and vice versa) will experience a change in seasons as well as possible fatigue from a long flight. In addition, the noise level on a plane, the dryness of the cabin air, other irritants that may be present in the cabin environment and the physical inactivity of a long flight all contribute to heightened fatigue. Avoiding alcohol and caffeine and using a sleep aid or melatonin may help mitigate this problem. It is a good idea to build extra time into your schedule so you can rest after long flights.
When sitting in a cramped airplane seat for a long time, some travelers might experience a serious condition known as deep vein thrombosis (DVT) or develop blood clots in their legs. Learn more about DVT.
Finally, simply due to happenstance given the billions of people who fly each year, just about any sort of medical emergency may occur on board a plane. If an incident does occur, flight crew members have first-aid training — though they’re not experienced medical personnel, and the equipment available to them is limited.
Some airlines check for visibly sick passengers in their waiting areas and during the boarding process. If you look like you may be sick, keep in mind that you may not be permitted to board.


In the United States, automobile crashes are a leading cause of death among people younger than 54 years of age. The most important way to improve safety when traveling in a motor vehicle is to wear a seat belt.
Source: cdc.gov
35,092
U.S. Motor Vehicle Deaths (2015)
Although infectious diseases receive a lot of attention, the major cause of disability or loss of life among travelers is motor vehicle crashes. A variety of factors contribute to motor vehicle crashes, most of which can be prevented or abated. These factors are well known and similar in all countries — the primary consideration is seat belt usage.
If you are the driver, reduce your chance of injury by familiarizing yourself with local traffic laws and cultural driving patterns before getting behind the wheel. Be aware that in some regions the local population may have limited observation of traffic laws with which you are familiar.
Know which side of the road to drive on, and plan to the extent that you can so you know the route you’ll be taking. Most modern GPS devices are preloaded with global maps, so if you own a GPS, check to see if you can use it in countries where you will be traveling.
The risks of a motor vehicle accident are likely to be greatest in developing nations due to poor road infrastructure, the disrepair of many vehicles, a modest culture of safety, and limited or inaccessible medical care. Remote locations may not have local emergency medical providers or a level of care sufficient to meet the needs of a seriously injured traveler. In some areas, medical standards may be different from those of more populous areas. Remote regions of the world have their appeal, but it is worth considering these drawbacks as you make your travel plans.

Marine travel involves some general hazards as well as those that are specific to certain types of vessels, destinations and activities. Most seagoing travelers are aboard either large cruise ships or small recreational boats.

Travel on a cruise ship involves health hazards independent of your destination — associated simply with isolation, confinement and extended exposure to your fellow passengers and the crew members, who may be carrying communicable diseases. Outbreaks of chickenpox and rubella (German measles), for example, have been reported on cruise ships. The most common shipboard outbreak is vomiting and diarrhea caused by noroviruses. Respiratory infections and foodborne poisonings are also common on cruise ships, as are lifestyle disorders due to dietary changes, overeating and excessive alcohol consumption.
Regardless of your itinerary, make sure you are up to date on all vaccinations for diseases such as measles/mumps/rubella, varicella (chicken pox), tetanus, seasonal flu and pneumonia.
Other cruise-ship hazards are related to being on a moving vessel and include motion sickness, falls that result in injuries and falls overboard that result in drowning.
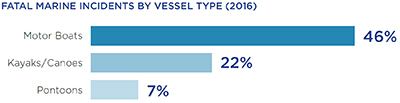
Health concerns for recreational boaters include injury, acute illness and other travel-related diseases. In 2016 there were more than 11.8 million registered recreational vessels in the United States alone. That year the U.S. Coast Guard logged 4,463 marine accidents, which involved 2,903 mandatory reportable injuries and 701 deaths. Most of the fatal injuries occurred on small vessels (26 feet or less). The types of vessels most often involved in fatalities included open motor boats (46 percent of incidents), kayaks and canoes (22 percent) and pontoons (7 percent).
Drowning was the cause of death in 80 percent of fatal boating incidents. Trauma and hypothermia were among the other causes. Of those who drowned, 83 percent were not wearing a life jacket. Alcohol use is a major contributing factor in fatal boating incidents and is listed as the leading factor in 15 percent of deaths. Other common risk factors include operator inattention, improper lookout, operator inexperience and excessive speed. Take steps to minimize or eliminate these factors whenever you set sail.
The most important thing you can do is to wear a life jacket. They really do save lives.
Medical rescues in remote locations, if even possible, are not covered by standard health insurance policies or Medicare. That’s why having a dedicated medical evacuation plan that covers you worldwide is smart protection.
200,000
EMERGENCY ASSISTANCE CALLS MADE EACH YEAR TO THE U.S. DEPARTMENT OF STATE
In some remote locations, rescue or evacuation services may be unavailable. All travelers, especially those headed to remote territories, should develop an emergency action plan (EAP) in case their trip goes off course. More than 68 million Americans travel abroad each year, and the U.S. government receives nearly 200,000 emergency assistance requests due to illness, injury or crime. The U.S. Department of State has assisted almost 11,000 families who have had a relative die during a trip.
The process of locating travelers in need of assistance, retrieving them and getting them to someone able to provide initial medical care is defined as the rescue phase of assistance.
If you are heading to a remote area, as part of your travel action plan be sure to have with you the contact numbers for a remote rescue service in the region where you’ll be traveling. Contact that service first if the need for a rescue arises.
Keep in mind that search-and-rescue operations can be quite expensive, so travelers to remote areas should carry search and rescue expense coverage. Even policies that cover rescues generally limit the amount they will reimburse, and they typically pay only organizations that are trained and approved to undertake search and rescue operations.

Medical evacuation is the transportation of an injured or sick person to the closest appropriate medical facility, such as a hospital or clinic, for assessment and emergency medical care.
Travel-assistance organizations optimize the evacuation process by balancing several factors: the type and urgency of the medical need, the available means of transportation and the proximity of facilities that can provide care. The patient will not necessarily be returned to his or her home country at this stage. Transportation methods used may include helicopters, airplanes, boats, ambulances or other motor vehicles.
Keep in mind that in some cases the cost of a medical evacuation — especially if it includes several stages and/or requires the use of a specialized air ambulance — can far exceed $100,000. Thus having a plan that covers medical evacuation is essential if you plan to travel to a remote area. Frequently, even if the traveler carries sufficient coverage, an evacuation may be delayed due to factors such as inclement weather or the unavailability of nighttime transport.
Medical repatriation is the transportation of an ill or injured traveler to his or her country of origin to receive medical care. Whereas medical evacuation gets you to the closest available medical care, medical repatriation transports you from that facility to another one back home.
If you become injured or ill while traveling and require hospitalization or a higher level of care, you may be returned to your home country if your condition warrants medical travel, if you are stable enough to travel and if the travel does not pose any additional risk to your condition. Your travel emergency-assistance provider will usually make such medical determinations in consultation with you and your treating physicians and then make all the necessary travel arrangements if repatriation is deemed advisable.
Planning for safe travel involves much more than securing your plane tickets and hotel reservations. Many hazards associated with travel — even to remote and dangerous settings — can be eliminated, or at the very least mitigated, by prudent planning. These actions are among the things you should do well before you leave home or even before you book your trip.
All travelers have a responsibility to themselves and to their traveling companions to research some basic facts about their destination. For example, knowing what the weather is like where you’re going — at the time of year you will be there — will allow you to pack clothing that will keep you safe and comfortable. Knowing the extent of local health precautions will help you determine what is safe to eat and drink and what items to avoid. This type of planning is an important first step in ensuring a great trip, whether to a favorite location or a brand-new spot.
How is your health? Has there been any change in your health status since your last trip? Are you seeing a physician before your trip to treat even a minor health issue? For example, a “simple” hernia could become entrapped and require emergency surgery where no such service exists. It is judicious to get your doctor’s approval for an upcoming trip and recommendations for maintaining good health during it. If you have activity limitations that would restrict the amount of walking, climbing or bicycling you do on your journey, you’ll need to factor that into your plans. Your abilities should match the type of lodging you choose and the means of transportation you’ll use during your trip.
Do you really know your medications — what drugs you take, the dosage and possible side effects? Certain medications can make you drowsy, more susceptible to acute mountain sickness or inattentive, while others can cause hypotension (low blood pressure), muscle pain, photosensitivity (an abnormal reaction to the sun), headache or other responses. These side effects can be annoying or, even worse, can increase your risk of injury during your travels. If you must start new medication before a trip, discuss with your physician when it will be safe to travel. In some countries, for certain medications you are required to carry with you an original prescription bearing your name and your physician’s signature. You may not be able to obtain any prescription medication or nutritional supplements you might need at your destination, so plan ahead.
Make sure to pack all appropriate health and safety-related necessities, but travel as light as possible otherwise. Hauling heavy luggage around may hurt your shoulders or back and spoil your trip. If you are flying, use your carry-on luggage for essentials such as your passport and other travel documents, medications, valuables and anything you need to travel in comfort. Try to limit your carryon luggage in number, size and weight so you can move expeditiously through airports and easily lift your bag into the overhead compartment. If possible, keep the space under the seat in front of you empty so you can stretch your legs. If you must walk for a long distance, try not to carry more than 10 percent of your body weight. Put a copy of your travel documents in each piece of luggage so you will still have critical information if one or more pieces are delayed or lost.
Purchasing travel health and medical evacuation insurance is highly prudent. Travelers are often responsible for hospital fees and other medical expenses they incur while abroad. Check your health insurance plan to see if it will cover your health needs abroad. Most domestic health insurance plans, including Medicare, do not. Even if you do have coverage, you should be prepared to pay out of pocket at the time you receive any medical services while you are traveling.
Before you leave home on a trip, especially if you are heading for a remote area or an undeveloped/underdeveloped country, make sure you know the signs and symptoms of common illnesses for the area in which you are traveling. This will prepare you to recognize them so you can act quickly in case of an emergency during your trip. The U.S. Centers for Disease Control and Prevention (CDC) website is a helpful resource for location-specific health information.
It’s always a good idea to be sure that at least one person back home has all the details of your itinerary and knows how to reach you — including where you would likely be taken in case of a medical emergency. The U.S. Coast Guard's Float Plan Central resources are especially helpful to boaters.
It is always wise to seek medical advice before a trip rather than assuming a health problem will not occur or figuring you are willing to accept the risk. Certain circumstances require planning ahead — and doing so can save you hassle and time and may even prevent some illnesses from occurring or worsening.
For a healthy person, the stress of travel may be exhausting but is unlikely to cause major harm. If you are healthy and fit, regular wellness visits to your doctor, such as annual physicals and screenings as suggested for your age, may suffice. If you have any preexisting conditions, have recently suffered an injury or acute illness, lead a sedentary lifestyle or have not had a medical checkup in a while, you should schedule a pre-trip health check with your primary-care physician.

The healthiest travelers are those who see their physician on a regular basis, take their medication as prescribed, eat nourishing meals and engage in regular exercise.
Of special concern for travel are illnesses that affect the pulmonary system, immune system, hormonal system, central nervous system or locomotive system, which can limit travelers’ ability to cope with the physical and mental stresses of travel. Women in advanced stages of pregnancy as well as newborns and infants require particular consideration.
Adventure travel and participation in some sports such as scuba diving involve additional demands on a traveler’s health. Depending on your destination, you may be asked to present a written medical assessment proving your fitness.
Before you begin a trip, develop a health maintenance plan, carry a list of the medications you take (including dosage) and when you take them, limit your intake of caffeinated beverages and alcohol, and drink water during and between meals to maintain a healthy level of hydration. The healthiest travelers are those who see their physician on a regular basis, take their medication as prescribed, eat nourishing meals and engage in regular exercise.
Individuals who take prescription medication and plan to travel abroad may be required to carry a letter from their attending physician describing the nature of their medical condition. Your doctor can also provide you with an explanatory note if, for example, you need to carry epinephrine pens or syringes and/or injectable medications such as insulin while flying or crossing borders. Be sure to place this letter in your carry-on bag, wallet or purse, and always keep it with you.
Keep your medication in your carry-on luggage in case your checked luggage is delayed or lost (the same is true for eyeglasses and/or contacts — and it’s a good idea to pack an extra pair, too). If you travel abroad, leave medications in their original, clearly labeled containers; this includes over-the-counter pain relievers as well as prescription drugs. It may be easiest to place all your medications in a clear plastic zip-top bag so customs officials can easily view them. If you have been prescribed a controlled substance such as a narcotic, check with the foreign embassies of any countries you plan to visit to make sure such medication is considered legal in those places. As a redundant precaution, consider dividing your medication supply and keeping them in two locations (your checked luggage and your carry-on) in case one or the other is lost or stolen.
The U.S. Department of State makes available contact information for all countries that maintain embassies and consulates in the United States. It is a good idea to carry in your wallet or purse a list of your medical conditions and any known allergies to medications, foods and insect bites. Diabetics may want to consider wearing a “medical alert” bracelet. This information can be crucial should you fall ill while traveling.
After you leave home, there are some things you can no longer do to protect yourself and many things that are much harder to undertake. Here are some tips about steps you can take in advance to maximize your chance of having a safe, comfortable and enjoyable trip. These precautions are especially important if you plan to travel through or spend time in remote or wilderness areas or undeveloped countries.
Receiving appropriate prophylactic (preventive) treatment and behavioral counseling — perhaps even from a professional trained in travel medicine — can go a long way toward reducing your health risks. Remember that your disease exposure will vary, depending on your destination. Schedule the appointment at least four to six weeks before your departure, as you may need some vaccinations that must be given in a series or that take time to become effective. When evaluating the risks you’ll be facing, consider your lifestyle choices, preexisting conditions, medication regimen, where you will be traveling and what you will be doing.
Be sure to discuss with your physician any drugs you wish to take with you, and familiarize yourself with the generic names for these medications. Certain factors are associated with an increased risk of acquiring a travel-related illness, so it’s essential that you are honest with your physician. It is important to review with your physician your itinerary and planned activities to assess the specific risks associated with the given locations and pursuits. For example, a trip to certain regions raises your risk of contracting malaria. A bicycle trip increases the risk of a traffic accident. A mountain-climbing or trekking trip comes with a risk of altitude sickness, and a diving trip involves a risk of diving-related injuries. Your physician should also consider preexisting conditions and your lifestyle choices.
Vaccinations are a safe, reliable and effective way to acquire immunity against infection from many pathogens. Given that more than 90 percent of travelers are repeat travelers, you can consider vaccinations an investment in your future. A list of recommended vaccinations is given below.
This routine vaccine should be given to anyone older than 12 months who has never had chickenpox. It can be given in a combination vaccine that includes measles, mumps and rubella.
A new cholera vaccine is available in the U.S. for adults ages 18 to 64 who are traveling to an area of active cholera transmission.
This routine vaccine is first given to children at two months of age and continues throughout the lifetime, often in combination with pertussis and tetanus.
This routine vaccine is given to children younger than age 5. It is needed only in certain populations over the age 5, depending on medical history.
This routine vaccine is given to children between 1 to 2 years old as well to those people who are traveling in areas where the virus is more widespread and to certain at-risk populations. An immune globulin can also be given at certain times if needed.
This routine vaccine is given to children starting as early as birth. It is also given to some unvaccinated adult populations that are at risk for exposure.
This vaccine is recommended annually for children and adults. It is strongly recommended for certain populations.
This vaccine is recommended for those traveling for more than a month in areas where JE prevalent. Those who are traveling for less than a month but who will be outside much of the time might also benefit from the JE vaccine.
This routine immunization is given to children starting at 12 months old. Some adults, depending on original vaccination, may need a booster.
Certain adult populations and travelers to areas where the disease is endemic should receive the meningococcal vaccine.
Some unvaccinated at-risk adult populations should be immunized. It is routine for adults older than age 65.
This routine vaccination is first given to infants at 2 months old. Unvaccinated adults who are traveling to areas where polio is common may need vaccination.
People at risk of exposure or who are traveling to areas where rabies is common should be vaccinated.
This routine vaccination is first given in infancy and is continued throughout the lifetime. It is often combined with diphtheria and pertussis vaccines.
This vaccine is recommended for travelers to areas where typhoid is common. Safe food and water handling is imperative.
This vaccine is strongly recommended for travelers to areas where yellow fever is endemic. Some countries may require the vaccine prior to entry.
Although the purified protein derivative (PPD) skin test is not an immunization, it should be considered to document tuberculosis exposure status.
Keep in mind that it’s a challenge to offer generalized vaccination recommendations and that thorough recommendations are beyond the scope of this guide. While the vaccination list will give you a sense of the important issues to consider regarding vaccines, you should carefully review your immunization status with your physician well before your departure date. Pay attention to routine vaccinations such as tetanus and diphtheria (DTaP/Tdap), measles (MMR), polio, hepatitis B, chickenpox (varicella) and influenza. The PPD test for tuberculosis exposure is also advised. Yellow fever is the only vaccination currently required by the World Health Organization (WHO), but some individual countries require proof of cholera vaccination. Other recommended vaccinations will depend on your itinerary, lifestyle and the length of your trip.

Visit the CDC for more information about recommended vaccinations for travelers.

You can check with the DAN Boater Medical Information Line, the CDC website or your doctor for the most up-to-date recommendations on vaccinations and other health-related issues.
The website of the U.S. Centers for Disease Control and Prevention (CDC) is a highly reliable source for the latest information on vaccination recommendations and location-specific health information. Information on the CDC website is available in several formats, so you can load pertinent resources onto your phone or other electronic device before you leave home.
In addition, the CDC has developed a series of free mobile apps that can be a great resource for travelers. Here is a brief look at a few of the apps.
TravWell is an all-in-one app that helps you prepare for your trip by offering location-specific vaccine and health information and by storing checklists, packing lists, medication records and travel documents. The app also provides a built-in alarm that reminds you to take medications or vaccine boosters. This can be helpful when you’re traveling in an unfamiliar time zone.

The Can I Eat This? app offers travelers peace of mind when trying new, unfamiliar food and drink by helping you avoid foodborne illness. Many travelers know how unpleasant diarrhea can be and will ruin any trip. Avoid food-related illnesses, and be more confident in choosing the right food and drink wherever you are. Just enter your location and the food or drink you want to try, and this app will tell you whether or not it’s likely to be safe.
The CDC’s Vaccine Schedules app offers quick access to the federally recommended immunization schedules, complete with detailed footnotes. Intended largely for healthcare professionals who recommend and administer vaccinations, this app may also be useful to health-literate laypeople.
The CDC’s Tickborne Diseases of the United States app serves as a quick reference guide for doctors and other health-care providers who may need to diagnose and treat tickborne diseases. Whether you are likely to encounter ticks frequently or only rarely, this guide may be of assistance.
Updated 2018-06-22: The CDC has discontinued the Tickborne Diseases of the US app.
In addition, the CDC publishes a biennial guide called CDC Health Information for International Travel, popularly known as the “Yellow Book.” This publication offers immunization guidelines and detailed travel health information; it is aimed primarily at health-care professionals, but it can be a useful resource for anyone interested in healthy international travel. The book is available online and as an app for Android and iOS mobile devices. A print edition is available from Oxford University Press.
An abundance of useful information is available on a variety of platforms. If you decide to strike out on your own online, keep in mind that nonprofit, academic and governmental websites are likely to contain the most reliable information; in the United States, such sites have domains ending in .org (for nonprofits such as DAN Boater), .edu (for academic institutions) or .gov (for governmental agencies).
Here are several additional sources of well-researched, dependable travel health information:
You may be traveling where you will have ready access to online resources. But if you will be spending time off the beaten path, especially if you’ll be engaging in risky sports, it is prudent to carry a comprehensive printed travel medical guide with you. See below for some suggested titles.

Since its inception in 1980, DAN® has spent more than 300,000 medical resource hours on duty, fielding more than 100,000 emergency calls and coordinating more than 10,000 emergency evacuations worldwide, making it one of the world’s most trusted resources for traveler safety.
As a natural evolution of DAN’s successful 35+ years of service to the diving community, our new DAN Boater Travel Safety Association is committed to helping recreational boaters and global travelers in need of emergency assistance while on the go, and to promoting smart travel health and safety practices through research and education.
By boat, plane, car, or rail. Around the world, or across the state. Anytime you travel more than 50 miles from home, rely on DAN Boater for the assistance you need when you need it:
Find out how our affordable annual travel safety memberships help travelers like you and your family every day.