

Imagine sailing across the crystal-clear blue waters of the Bahamas when you suddenly face-plant on a slippery deck and dislodge a tooth. Or, picture waking up in the middle of the Indian Ocean with a throbbing toothache that over-the-counter pain meds won’t touch. Ouch!
Dental emergencies can happen at any time—even when hundreds of nautical miles separate you from home and your trusted family dentist. And more than an inconvenience, they can be painful, stressful, and, at times, a danger to your health.
According to a French study published earlier this month, dental emergencies occurring most frequently on water range from dental abscesses (51.8%) and tooth decay (33.3%) to dental fractures (8.9%)—all of which can be problematic with no special equipment or dental specialists on board.
What’s more, a recent pilot study led by Vinisha Ranna, DDS, at the University of Buffalo in New York, found that recreational scuba divers may indeed experience dental symptoms during a dive. The study's results, which were published in the British Dental Journal in November 2016, indicated that most of the problems reported were due to barodontalgia, an acute toothache caused by the increase in pressure underwater. But study participants also reported jaw and dental pain caused by clenching the regulator mouthpiece too tightly, as well as loosening of crowns and gum pain.
Today we're going to show you how to prevent and manage dental emergencies at sea, step by step.

To do that, we spoke with Herb Benavent, DDS, a dentist and avid sailor who, in 2017, took time off from his family practice in Maryland for a multi-year sailing adventure with his artist wife, Maddie, aboard their Morgan 45 sailboat, Wisdom.
Let's get started:
** This website does not provide medical or dental advice. See additional information. **

A major cause of dental emergencies at sea stems from the fact that most folks fail to receive proper dental care before casting off. In fact, the French study suggested that most dental dilemmas could be avoided by a pre-trip checkup.

Even after taking the proper precautions by visiting your dentist pre-departure, you may still experience a dental emergency on board. All yachties should have an easily-accessible first aid kit but here's a list of extra items you'll need for handling for dental issues:

Don't let a toothache ruin your trip.
If you encounter a dental emergency while underway, you're in good hands with DAN Boater. Call our Medical Information Line for help locating dental services near you.

Just because you’re sailing or cruising doesn’t mean you get a break from your oral hygiene routine. To avoid potential damage to your smile, be sure to:

Cavities don’t form from bacteria eating your teeth; they form from bacteria eating the food you eat and producing lactic acid as a byproduct of their metabolism. In fact, they live and eat on your tooth, and this lactic acid that is excreted from them is what causes tooth decay and cavities to form. At home, you have your diet and routine, and this works well at controlling the bacteria in your mouth that live on your teeth. When you travel, however, your routine is upset, and you’re adding new foods to your diet. This means that new bacteria will start to colonize, and they may not be swept away by the same healthy habits you stick to at home.
The stress of traveling can also change the quality and quantity of your salivary production, which in turn, can change the environment in your mouth drastically. To help keep cavities at bay while at sea, make a point of:

From a throbbing toothache or lost filling or crown, to a chipped tooth or an accident that knocks your tooth out, here’s how the handle the most common dental dilemmas you may encounter at sea:
These can be caused by decay, fractures, infection or trauma. Rinse your mouth with warm salt water, and take 800mg of Ibuprofen every 6 hours for the first day and a half (6 doses), then every 8 hours until the pain has subsided. Seek immediate emergency help if something broke off your tooth or a part of your tooth is visibly missing, or if there is a “pimple” on the side of your gums, which is a draining abscess. If nothing is visibly missing, or different, seek emergency help if the pain is still there after 2 days of Ibuprofen.
Teeth can break for no reason and with no warning. It might not be the last bite that you took with that tooth that caused it to break, but instead the lifetime of chewing that culminated in the catastrophic failure of the tooth. When a tooth breaks, it will either be a small chip that doesn't expose the underlying layers, or it will be a deep fracture that will open up the deeper layers of the tooth.
If the chip is only in the enamel, take some Ibuprofen to help with any sensitivity that might occur, but the tooth doesn't need any immediate treatment. If the chip is deeper and goes into the dentin (yellow layer), then you might have more sensitivity. Placing Cavit over the exposed tooth will help shield it from the elements and will allow the nerve some protection. Cavit will have trouble staying put, however, and will probably need reapplication every few days.
If the chip is very deep and exposes the pulp—and the pulp is bleeding— place Cavit directly onto the hole and cover up the fractured area as best you can. Once that’s in place, begin taking 800mg Ibuprofen for the pain that will follow, and begin searching for immediate professional dental care. If the pulp is not bleeding, or even looks like a black hole, do not cover the chipped tooth. This indicates that the nerve is dead and gone. Bacteria in the pulp space can build up pressure and cause the tooth to break. The hole is now acting as a vent and will provide a way to release the pressure and therefore release the pain that would develop from this situation. If you cover the hole, you will build pressure in the tooth, and intense pain can ensue. You want to seek prompt dental care to get this tooth fixed, but you are going to need a root canal, so make sure you are in a country that is known for good dentistry.
If a tooth gets knocked out, you need to put it back in the socket as quickly as possible. Rinse the tooth off with sterile water or milk to remove any debris from the tooth, then shove it back into the socket. Make sure you orient the tooth properly, because the tooth will most likely fuse to the bone and get stuck this way permanently. If you don't feel comfortable putting teeth back where they belong, the next best thing is to put the teeth in milk. Do not rinse them off or scrub them, just leave them to soak. For both situations, seek immediate dental care.
This will look like a pimple on the side of your jaw or in your gums. You need to drain this by popping it and letting all the puss out, then immediately begin taking antibiotics. (Amoxicillin 500mg three times daily, or Clindamycin 150mg four times daily). As long as the infection has a way to drain itself, pressure will not build, and the pain will not be unbearable. You don't want to cover or try to get the abscess drain hole to close.
If the abscess is near the gum line, this is caused by something that got stuck in your gums. Take a dental pick and sweep the area. Orient the pick in line with the side of the tooth, aiming into the gums, and slip the tip of the instrument between the tooth and the gums. You might see a little bleeding while you do this, but it should be minimal. If you see a lot of bleeding, you are doing it incorrectly and causing trauma to the tissue. Stop what you are doing and seek the help of a dental specialist.
The dental pick should pull out whatever was stuck down there and also dislodge the abscess, which will cause a lot of puss to emerge. Puss is usually white, but sometimes it can be a creamy yellow color. The goal is to get the puss out so that the gum lays flat against the tooth again. The foreign object might not be found because it could have slipped out before you got in there. These should heal and swelling should go down on its own without requiring the use of antibiotics.
If the tooth has a root canal, there is no nerve and you will suffer no discomfort without your crown present. If the tooth does not have a root canal, it will be sensitive to cold until the crown is recemented. Hold onto your crown and take it to a dentist as quickly as you can to have it recemented. Teeth will begin to move, and the space the crown used to fit in will close up, making it difficult to place the crown in a few days. If you can't get the crown put on within 24 hours, then you can put it on with some temporary cement.
If you have no temporary cement handy, you can use tooth paste to help hold the crown in place. Either way, the secret is to dry the tooth off as best you can before you put the crown back on. The drier the tooth, the firmer the hold.
If the edges of the wound are adjacent to each other, then it should heal on its own without sutures. If there is a gaping gash, and someone on board has the skills to suture a wound, that would be ideal. If that’s not possible, seek immediate care, because a gaping gash that is remaining open requires stiches. Even if you can’t get immediate medical attention, the wound will heal—just much more slowly and with a bit of scarring.
Regardless, you need to control the bleeding by putting pressure on the wound with gauze. If the bleeding comes to a slow trickle in a few hours, it can be allowed to heal on its own. Otherwise, keep pressure on the wound until you’re able to get emergency care.
Special Note for Divers on Barodontalgia
Barodontalgia is more commonly caused with resin restorations (white fillings), because tiny air bubbles can be trapped in the resin when the filling was placed, and these tiny air bubbles will be subject to pressure changes. Amalgam (silver fillings) will not have these air pockets, because the liquid metal is compacted into the tooth, fully expelling any air pockets that could have existed.
Divers can avoid jaw pain by not biting down on the mouth piece with force during the dive. Putting excessive force on your teeth and jaw for an extended period will cause pain, and the only way to prevent it is to loosen up. Dr. Benavent advises viewing it as the mouthpiece being in your mouth giving you air, with your lips and teeth merely guiding it in place. If you loosen up on the mouthpiece, the regulator won’t fly out of your mouth, and your teeth and jaw will thank you.

When do-it-yourself measures aren’t working, or you don’t feel comfortable or confident in managing a dental problems on your own, you need to take action. If you’re close to land, go ashore and find the closest medical or dental facility. If landfall is not possible, try calling your dentist. He or she may be able to help guide you to a temporary fix by phone or Skype until you can get further treatment. If you need immediate attention, ask your dentist for a referral in an area you’re closest to—or, if out of the country, check the U.S. embassy or consulate office for recommendations.
Better yet, secure a DAN Boater membership before departure. In addition to providing emergency medical evacuation services, DAN Boater can also help you with dental and medical referrals where you're traveling.
Finally, invest in a travel insurance policy that includes coverage for dental treatment so you’ll have the protection you need—just in case.
MORE FROM
SAFE PASSAGE
TRAVEL HEALTH | Aug 31, 2018
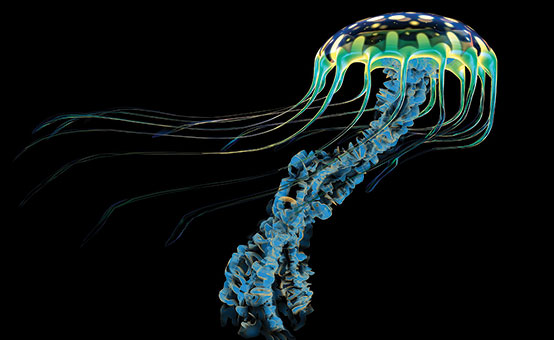
First Aid for Hazardous Marine Life Injuries (Guide)

TRAVEL HEALTH | May 24, 2018
How Long Does Seasickness Last? (video)
THIS WEBSITE DOES NOT PROVIDE MEDICAL OR DENTAL ADVICE.
It is intended for general informational purposes only and does not address individual circumstances. It is not a substitute for professional medical or dental advice, diagnosis or treatment and should not be relied on to make decisions about your health. Never ignore professional medical or dental advice in seeking treatment because of something you have read on the DAN Boater website. If you think you may have a medical emergency, immediately call your doctor, dial 911, or contact emergency services nearest you.